A “revolutionary” method to treat severe acid reflux has been implanted in patients for the first time, which could help tackle an issue that impacts 20% of the UK’s adult population.
University Hospital Southampton (UHS) and Imperial College London have become the first NHS trusts in the country to install the device called the RefluxStop, with Southampton being the first to use robotic surgery for the procedure.
Known as gastro-oesophageal reflux disease (GORD), the condition occurs when contents from the stomach flow back into the oesophagus – the long tube that carries food from the throat to the stomach.
It happens when the muscular valve – the lower oesophageal sphincter – at the bottom of the oesophagus becomes weakened because it has moved too close to the diaphragm or even into the chest which affects its function to allow food in and stop acid leaking out.
This can result in a range of symptoms including heartburn, regurgitation, difficulty swallowing, bloating, excessive salivation, coughing, nausea and a hoarse voice, as well as teeth and gum damage, nutritional problems, and sleep impairment.
RefluxStop is fixed to the upper part of the stomach wall and blocks movement of the lower oesophageal sphincter to hold it in its original, natural position and restore normal anatomy and function.
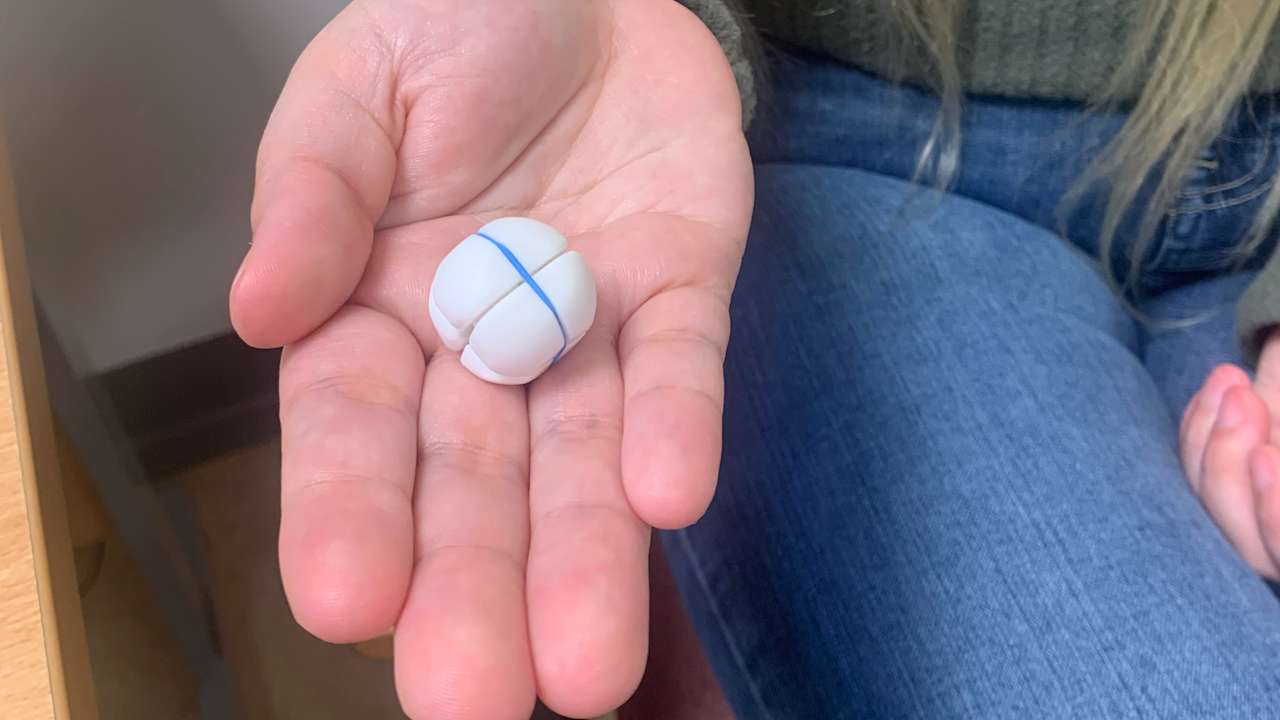
Made out of medical grade rounded solid silicone, the implant measures around 25mm – smaller than a ping pong ball – and is fitted via robotic-assisted laparoscopic (keyhole) surgery as a day case, with patients in theatre for less than two hours.
A UHS spokeswoman said that approximately 20% of the adult UK population have problems with severe acid reflux or GORD and UHS treats about 50 patients every year with the condition.
The disease can also lead to further complications such as oesophageal ulcers, a scarred and narrow oesophagus, Barrett’s oesophagus – changes to the cells in the lining of the oesophagus – and oesophageal cancer.

It is estimated that one in every 10 to 20 people with Barrett’s oesophagus will develop oesophageal cancer within 10 to 20 years.
Danielle Harding, 30, recently became the first patient with GORD to undergo the procedure at UHS.
The mother-of-two, from Southampton, said: “I began suffering with severe acid reflux in 2022 and it has affected my life in so many ways – anything that involves eating or drinking has caused me so much anxiety, especially outside of my home.
“The signs are almost immediate with an intense pain in my chest as the reflux comes up the oesophagus and burns my throat, often resulting in me vomiting, it’s been horrendous.”
Ms Harding was prescribed medication from her GP which initially stopped the symptoms only for them to return.
An endoscopy showed that she had significant damage to her oesophagus and that she would need to remain on a high dose of medication for life.
Ms Harding said the RefluxStop was a “no-brainer” for her and added: “I had the surgery a little over a month ago and my symptoms have completely disappeared.
Fergus Noble, consultant general and oesophagogastric surgeon at UHS, said: “RefluxStop is revolutionary in that it is minimally invasive, restores the lower oesophageal valve to its natural position with no side effects and offers some patients a viable treatment option for the first time.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country





























