Key findings in the report
-
 UK Government promises ‘comprehensive compensation’ to those affected
UK Government promises ‘comprehensive compensation’ to those affected -
 Prime Minister Rishi Sunak has apologised to the victims of the infected blood scandal and their families
Prime Minister Rishi Sunak has apologised to the victims of the infected blood scandal and their families -
 UK blood services failed to ensure sufficiently rigorous donor selection and screening of donors
UK blood services failed to ensure sufficiently rigorous donor selection and screening of donors -
 Transfusions were frequently given in situations where they were not clinically needed
Transfusions were frequently given in situations where they were not clinically needed -
 The UK failed to achieve self-sufficiency in blood products
The UK failed to achieve self-sufficiency in blood products -
 Commercial factor products were unsafe and should not have been licensed for use in the UK
Commercial factor products were unsafe and should not have been licensed for use in the UK -
 Doctors treated patients with increasing volumes of factor concentrates despite the known risks of viral transmission
Doctors treated patients with increasing volumes of factor concentrates despite the known risks of viral transmission -
 The UK Government failed to take steps to address risk that cause of AIDS could be transmitted by blood and blood products
The UK Government failed to take steps to address risk that cause of AIDS could be transmitted by blood and blood products -
 Patients were tested for both HIV and Hepatitis without their knowledge
Patients were tested for both HIV and Hepatitis without their knowledge
Thousands of people had their lives destroyed after receiving infected blood in a treatment disaster that has been described as “no accident”.
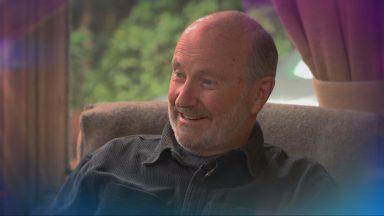
Sir Brian Langstaff, the chair of the Infected Blood Inquiry, published his report on Monday into a catalogue of failures by those in authority and repeated his call for compensation to be paid to those affected.
The inquiry found deliberate attempts were made to conceal the disaster, including evidence of Whitehall officials destroying documents.
The probe also found patients were knowingly exposed to unacceptable risks of infection.
Prime Minister Rishi Sunak apologised to the victims of the scandal and their families in a statement to the House of Commons, saying: “I want to make a whole-hearted and unequivocal apology for this terrible injustice.”
Sunak promised to pay “comprehensive compensation” to those affected and infected by the scandal.
“Whatever it costs to deliver this scheme, we will pay it,” he added, saying details would be set out on Tuesday.
He said: “This is a day of shame for the British state.
“Today’s report shows a decades long moral failure at the heart of our national life – from the National Health Service to the civil service, to ministers in successive governments, at every level the people and institutions in which we place our trust failed in the most harrowing and devastating way.
“They failed the victims and their families and they failed this country.”
The 2,527-page report documents a “catalogue of failures” which had “catastrophic” consequences, not only among people infected with contaminated blood and blood products, but also their loved ones.
Tens of thousands of people in the UK were infected with HIV and/or hepatitis after they were given contaminated blood and blood products between the 1970s and early 1990s.
Ministers have earmarked around £10bn for a compensation package for those affected, which is expected to be announced on Tuesday.
 Getty Images
Getty ImagesSir Brian said: “In families across the UK, people were treated by the NHS and over 30,000 were given infections which were life shattering. 3,000 people have already died and that number is climbing week by week. Lives, dreams, friendships, families, finances were destroyed.
“This disaster was not an accident. The infections happened because those in authority – doctors, the blood services and successive governments – did not put patient safety first. The response of those in authority served to compound people’s suffering.
“The government is right to accept that compensation must be paid. Now is the time for national recognition of this disaster and for proper compensation to all who have been wronged.”
Sir Brian’s report found that patients were knowingly exposed to unacceptable risks of infection.
It states the risks of blood and blood products causing severe infection were known well before most patients were treated: in the case of hepatitis since the end of World War Two.
The report states: “Government decision-making was slow and protracted. ‘Doctor knows best’ was such a strong belief that health departments did not issue guidance to curb unsafe use of blood and blood products.
“Doctors lost sight of what was known about the risks of viral infections from blood. Treatment practices that could have reduced the risk were not adopted.
“Patients were not informed of the risks of their treatment and were thus denied their rightful choice. They were tested without their knowledge or consent and not informed of the result, sometimes for years.
“Some people treated with blood products, including children, were further betrayed by being used in medical trials without their knowledge or informed consent.”
Who is affected by the infected blood scandal?
Two main groups of victims are affected by the scandal – people who needed blood transfusions and people with bleeding disorders who needed blood, or blood products, as part of their treatment.
People need blood transfusions for a wide variety of reasons including routine surgery, as a result of childbirth or if they have been in an accident or had an injury where they have lost a lot of blood.
Many victims had bleeding disorders, particularly people with the condition haemophilia.
Haemophilia is an inherited disorder where the blood does not clot properly. Most people with the condition have a shortage of the protein that enables human blood to clot, known as Factor VIII.
In the 1970s, a new treatment was developed – factor concentrate – to replace the missing clotting agent, which was made from donated human blood plasma.
Manufacturers made the product by pooling plasma from tens of thousands of people – increasing the risk of the product containing blood infected with viruses including hepatitis and HIV.
People with haemophilia were treated with British and American blood products.
A shortage of UK-produced factor concentrate meant clinicians relied on imports from the United States, where people in prisons were paid to be donors, despite being at higher risk of carrying infection.
Scots among those seeking the truth
 STV News
STV News
Bruce Norval from Inverness was diagnosed aged 23 with Hepatitis C from contaminated blood products.
He told STV News there is still an assumption that victims are partly responsible for their infections.
“I was three. Some of the boys were three months old,” he said. “Some of the HIV victims never even got to be here. We had babies dying at three years old.
“This wasn’t our fault and the people that did it to us, knew they were doing it to us but we’ve had to carry the can for decades.
“Yet most people still live hand to mouth in unsuitable housing, with inadequate care, with inadequate support, frequently without anybody around them, even knowing why they’re ill and still having to live in secrecy because of the fear and the bigotry of others.”
 STV News
STV NewsBruce hopes the inquiry’s final report will improve societal attitudes to those affected by the blood scandal.
“I have gone through an awful lot in the last couple of weeks waiting for the inquiry findings,” he said. “I thought that I had insulated myself against it, but in the last two weeks I’ve cried a lot. I’ve got angry. I’ve got upset.
“I’m finding myself getting a bit manic because I’m second guessing myself in relation to the evidence I gave to the inquiry – and the other evidence that I know that should be exposed by the inquiry – and the implications of that.
“The fact that governments held out for over a year after the compensation recommendations hasn’t helped because there’s no certainty in our lives.”
Former teacher and author Gill Fyffe is another Scot affected by the scandal. She has severe sensitivity to light following experimental treatment for Hepatitis C.
The consequences of that and of a transfusion given to her in 1988 following complications after childbirth continue to this day.
 STV News
STV NewsShe said: “The doctor kept saying ‘but the blood is 100% safe’. Then he invited a consultant from the blood transfusion service to come and talk to me and he said it was 100% safe.
“We now know at that time everybody knew it wasn’t and that there was a problem with the blood supply.
“Lots of families have become broken. This happens to people indiscriminately and some people can’t cope with it. It’s not fair, you’re not meant to be able to cope with something like this.
“So I think there should be compensation because I think it should give back what has been taken away. I don’t see it as a reward.
“I now have four grandchildren and another one on the way. I love it. I am the luckiest granny. They are all adorable. My favourite thing is when they all get together. This room does not look like this when they’re all together.
“The things that are important in life have not been taken from me which is why I am smiling. I massively feel for the people…there are some really sad stories at the inquiry. Every time we go we are all crying. Life goes on doesn’t it.”
Scottish Government ‘reiterates sincere apology’
The Scottish Government on Monday welcomed the report and said ministers have established an Oversight Group to consider the recommendations for Scotland.
Public health minister Jenni Minto said: “I welcome the Infected Blood Inquiry’s report and thank the Inquiry Chair and staff for their work in producing such a comprehensive final document.
 STV News
STV News“Today is about those who have been infected, their families and support organisations and I want to pay tribute to them. They have been focussed on ensuring the impact of this terrible tragedy, their suffering, has not been ignored. On behalf of the Scottish Government, I reiterate our sincere apology to those who have been infected or affected by NHS blood or blood products.
“The Scottish Government has already accepted the moral case for compensation for infected blood victims and is committed to working with the UK Government to ensure any compensation scheme works as well as possible for victims.
“The Scottish Government has set up an Oversight Group to consider the Inquiry’s recommendations for Scotland. That group will involve senior staff from NHS Boards and the Scottish Government, along with charities representing the infected and affected.
“We are determined to use the Inquiry’s report to ensure lessons have been learned so a tragedy like this can never happen again. However the Scottish National Blood Transfusion Service has extremely high standards of blood safety and I would continue to encourage anyone who can do so to give blood, as this remains essential for thousands of patients.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country