Inspectors have raised “significant concerns” about the culture at a children’s psychiatric hospital in Glasgow, with some patients reporting feeling “belittled and bullied” by staff.
An inspection of Skye House, a 24-bed specialist unit in the north of the city, found some staff “could not be relied upon to be compassionate or empathetic” towards patients with conditions including depression, psychosis and eating disorders.
One patient reported being told she was “pathetic” and “selfish” for needing to be fed using a nasogastric tube.
Another said that if she self-harmed, some nurses would not clean blood from her face before walking through the ward area to the treatment room.
The inspectors said they were given the impression that a “minority of staff” believed some patients “chose to behave in the way they did” and were “less deserving of the care”.
They added that this appeared to be particularly the case where young people had several admissions to the facility.
The joint inspection by Healthcare Improvement Scotland (HIS) and the Mental Welfare Commission for Scotland (MWC) was carried out in August, after a 2025 BBC documentary featured allegations of a “culture of cruelty” at the hospital.
Staff ‘burnt out’
In light of the allegations, then-social care minister Maree Todd commissioned the bodies to visit all three young people units in Scotland, and the separate children’s in-patient psychiatric unit in Glasgow.
The unannounced visit to Skye House saw the inspectors review health records and engage with 22 patients, 15 staff, and the relatives or carers of 19 patients.
Their report, published on Thursday, also raised several other concerns about the hospital.
These include a “significant issue” with staffing levels at the facility, with some staff reporting feeling “burnt out” as a result of the pressure they are working under.
The inspectors found nursing staff are regularly working additional hours, and that there is a reliance on “bank” staff or staff from adult wards, who it was said “did not understand how to interact with teenagers”.
The report also raised concerns about the way the use of restraint by staff was being recorded, but found all recorded instances of restraint were “proportionate to the level of risk being managed”.
 STV News
STV NewsAt the same time, the inspectors found a number of areas of good practice, including observing “positive, respectful and responsive interactions” between patients and staff, and the sourcing of additional funding to address the long-standing staffing issues.
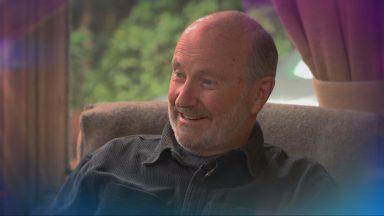
Claire Lamza, executive director for nursing of the Mental Welfare Commission for Scotland, said while there was some positive engagement with patients, some of the main concerns centred around staffing.
“What we did hear is that there was an issue that some of the staff in the unit had not had the full training they needed. There was a lot of bank usage in that particular period of time; these individuals weren’t part of a core team and don’t necessarily know how to support a young person who is stressed, dealing with a lot and whose behaviours result from that stress.
“There are still a few people concerned with the way the staff had approached them and some aspects of care and treatment, in terms of restrictions and not seeing doctors enough.
“We’ve known that there is a national issue with having enough registered nurses, consultant psychiatrists and mental health officers to ensure treatment delivered meets all legislative requirements. We know there is work being done, but at this point in time, we’re still concerned that it’s going to have an impact on care and treatment.
“We will continue to support NHSGCC and go out and visit and see these things are re put in place – particularly for young people, carers, and families – to make sure that what was being said in the past is something we can then challenge and say ‘this is what is happening now.'”
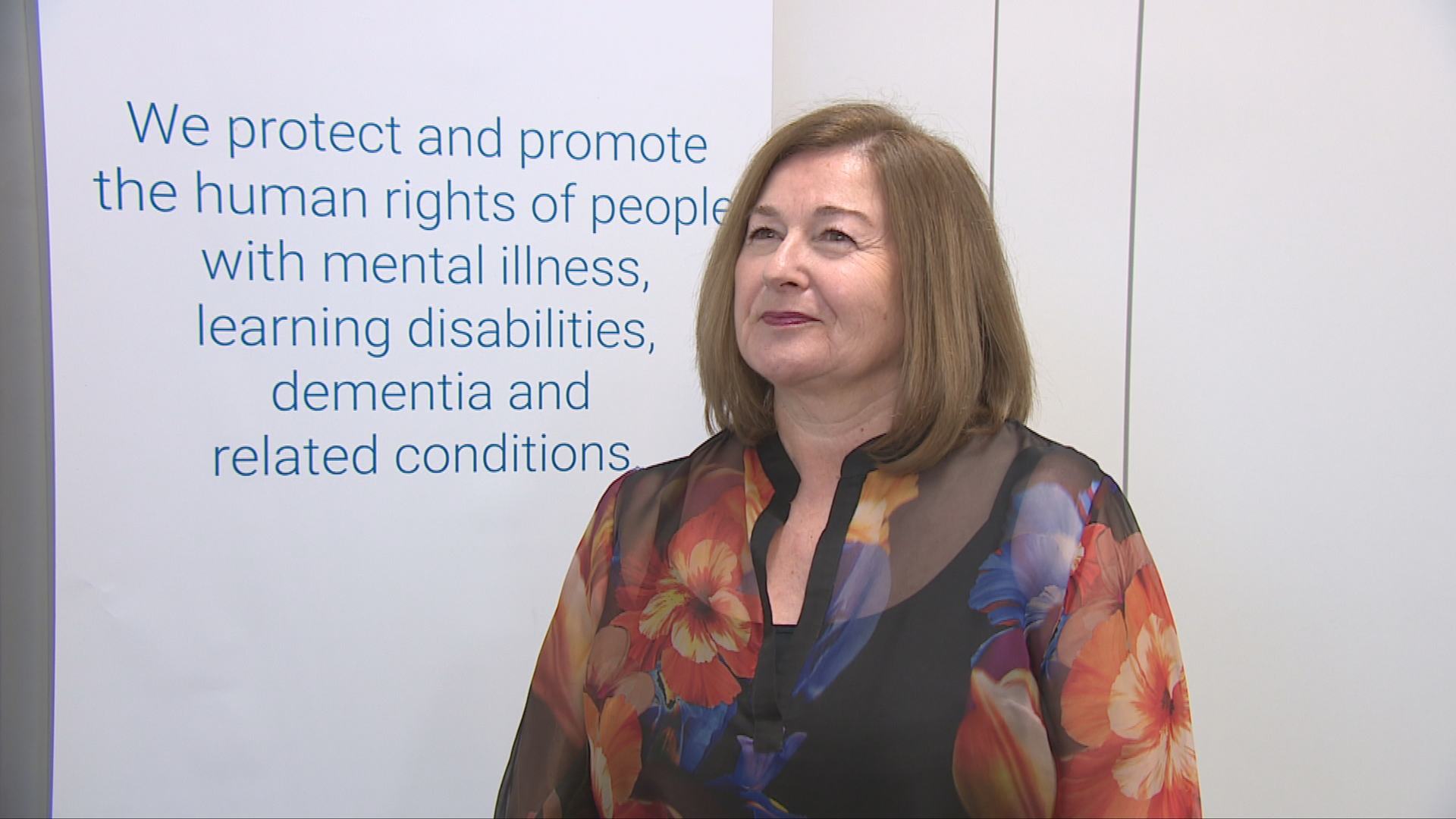
Robbie Pearson, chief executive of HIS, and Julie Paterson, chief executive of the MWC, said: “During this joint visit, Healthcare Improvement Scotland reviewed how the overall system of care is organised, while the Mental Welfare Commission focused on the direct experiences of young people and their families/carers.
“The report highlights the voices and experiences of young people and emphasises the need to strengthen and maintain a positive, respectful culture.
“It is essential that every young person consistently receives empathetic and compassionate care and that practice is fully compliant with the Mental Health (Care and Treatment) (Scotland) Act.
“We also saw positive examples of visible leadership, with a supportive environment for staff and examples of good practice.”
The report includes a list of 16 “requirements” for the health board, which it says are necessary for it to meet national standards.
Mr Pearson and Ms Paterson added: “We are confident that the requirements and recommendations are the right ones to ensure significant change in the care that young people receive.
“An improvement action plan has been developed by NHS Greater Glasgow and Clyde (NHSGGC) and we expect the NHS board to address the areas for improvement and prioritise the requirements to meet national standards.”
‘We accept that more needs to be done’
NHSGCC say changes include increased staffing, a reduction in beds from 24 to 16, the introduction of parent drop-in sessions and a dedicated parent group, along with building improvements.
An external review of the service has also been commissioned by the Royal College of Psychiatrists, with the findings due in March.
Derrick Pearce, Lead Director for Specialist Children’s Services at NHSGGC, said: “We consider it our responsibility and our absolute priority to ensure that children and young people have the right to feel safe, listened to and treated with dignity.
“Since we were made aware of issues, a significant programme of improvement work has been undertaken. This has been overseen by the Chief Officer for the service, alongside NHSGGC’s Medical Director and Nurse Director.
“This inspection took place at the mid‑point of the improvement plans to tackle the challenges facing the service, and the report highlights a number of improvements already in place, including strengthened leadership, additional oversight and changes in how care is delivered within the unit. However, we absolutely accept that more needs to be done to improve service provision.
“We have a dedicated focus on improving the service and continue to work closely with Healthcare Improvement Scotland, the Mental Welfare Commission, staff, young people and families, and wider CAMHS services to ensure the required improvements are delivered. This includes bringing forward a new model of service currently in development to better meet the needs of our children across a continuum of care, including intensive support in the community.
“We understand that patients and families may have questions or concerns following the publication of the report, and we are actively contacting them so that we can listen, explore concerns and provide answers.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country


 Google Maps
Google Maps