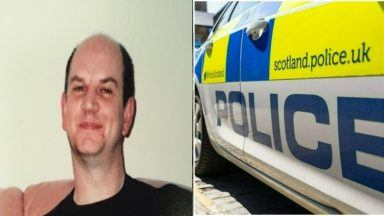
A health board has been ordered to issue an apology after nursing staff “consulted NHS24” for advice on how to treat a dementia patient who developed sepsis.
The Scottish Public Services Ombudsman (SPSO) has instructed NHS Lanarkshire to apologise to the patient’s child, referred to as C to protect their anonymity.
C’s parent, referred to as A, had a common form of dementia (vascular dementia) which affected their mobility, and was admitted to a community hospital following a fall.
C complained about the care and treatment that their parent received during an admission to a community hospital.
They told the SPSO that A had a number of falls in hospital and suggested that one of these falls led to an injury to their leg.
Alongside this, C also made complaints regarding the nursing care and implied that A was allowed to become dehydrated, only drinking when assisted by family members or when family members prompted the ward staff.
The patient’s child also raised concerns about the clinical aspects of their care, saying that their parent became lethargic and unresponsive during their admission to hospital.
Family members did express their concerns to staff that this may have been the result of sepsis (blood infection) or a urinary tract infection. However, they were reassured that A’s symptoms were likely caused by antibiotics.
A then suffered a heart attack, during which staff performed cardiopulmonary resuscitation (CPR) to revive them, after which they were transferred to a general hospital for care where A died five days later.
C explained that A was uncomfortable and agitated during their final days, and that staff there had expressed concern regarding the lack of a Do Not Attempt Cardiopulmonary Resuscitation (DNACPR).
The late patient’s child complained that the additional five days of suffering that they experienced could have been avoided had a DNACPR been discussed with family members.
The ombudsman found that A’s condition and medical history meant that clinical staff should have considered DNACPR each time that they reviewed them.
It also found that A had developed sepsis, likely as a result of the leg injury sustained during their admission, and noted a delay of several days before the cut to A’s leg was identified.
Once nursing staff became aware of this, they appropriately escalated the situation to the clinical team – but no clinical review was carried out, and the watchdog found that nursing staff instead “consulted NHS24 for advice as to how to treat A’s leg” and treated them with antibiotics.
The SPSO stated that had a member of the clinical team at the hospital performed an in person review of the severity of A’s condition, sepsis could have been prevented by intravenous antibiotics.
It noted an “overall lack of clinical input into A’s care during their admission” and concluded that this was the reason for the delay in a sepsis diagnosis.
With regard to the nursing care that A received, it found that there was a four-day delay to A’s falls risk being assessed and mitigated after their transfer to hospital.
The number of falls A had and the severity of the harm caused increased during this time, and it found that this was a “clear failure to adapt to a patient’s specific needs”. The SPSO was critical of the board for “failing to record and monitor A’s leg wound in a wound chart”.
It stated: “Whilst we were satisfied that there was evidence of the nursing staff monitoring A’s food and fluid intake, we noted that their focus was on the weekly variations in A’s weight.
“This meant that A’s significant weight loss over a longer period was not identified.
“Had it been, staff may have taken proactive steps to increase A’s intake and increase their weight. We upheld all aspects of this complaint.”
The SPSO ordered NHS Lanarkshire to apologise to C and the rest of A’s family for its failings. It also recommended that the board conduct a review of the nursing care provided on A’s ward, and take steps to ensure compliance with relevant standards.
It also recommended that the board conduct a review of the medical provision available to patients on dementia wards at the hospital and take steps to ensure that they meet the standards of inpatient care set out in the guidance from the Royal College of Psychiatrists.
The board was also asked by the ombudsman to share its decision with the nursing staff.
Judith Park, director of acute services, said: “We understand this has been an extremely difficult time for the family and our thoughts and sympathies remain with them.
“We regret any instance where we have failed to provide the highest standards of care for our patients.
“We have fully accepted the recommendations within the Ombudsman’s reports and will develop an action plan to address them. The lessons learned will be shared to help avoid similar occurrences in future.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country