A mum has described the “euphoric” moment she lifted her baby from her womb during a caesarean section in a procedure thought to be the first of its kind in Scotland.
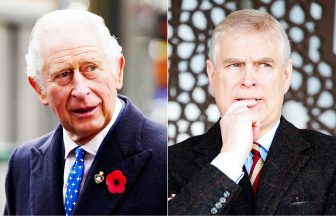
University lecturer Dr Leila El Alti gave birth to daughter Aurora by “maternal-assisted c-section”, which involves the mother effectively becoming part of the operating theatre team.
Leila described the moment she pulled her baby from her abdomen and onto her chest for immediate skin-to-skin bonding as “the most magical experience of my life”.
Ahead of the arrival of her daughter, the 39-year-old from West Lothian scrubbed her hands and forearms along with the doctors, nurses and midwives.
 NHS Lanarkshire
NHS LanarkshireShe also wore a surgical gown and gloves to prevent infection as she helped to birth 7lbs 9oz Aurora.
Speaking at an NHS Lanarkshire board meeting, Leila said: “I’d recommend it to any woman who feels they would benefit from having such an active and empowering role in giving birth by c-section.
“I felt euphoric for weeks after Aurora was born in March, and my joy was not just for myself – my having done this successfully has hopefully opened the door for other women to also have this wonderful experience as a valid birth option.
 NHS Lanarkshire
NHS Lanarkshire“I was anxious to have a maternal-assisted procedure to give me a vital sense of difference, empowerment and control because the caesarean births of my first two children were highly traumatic. I was prepared to go anywhere in the UK.”
Leila discovered that the health board already had a policy for “gentle method” c-sections.
This method doesn’t involve the mum’s assistance but includes a “holistic” birth experience with slower delivery, the woman seeing the birth and immediate skin-to-skin contact.
She explained: “I did a lot of work and research and, through social media, I found a woman in England who’d given birth the maternal-assisted way. I put her midwife in touch with the NHS Lanarkshire team, which helped them gain confidence and understanding of the procedure.”
 NHS Lanarkshire
NHS LanarkshireBecause she wanted to be involved in the decision-making process, Leila also sent a heartfelt audio recording to the team, outlining why she needed the procedure, and other key steps alongside it, to avoid being re-traumatised following the births of her first daughter, now aged seven, and her son, aged two.
Originally from Lebanon, Leila worked there as a registered nurse in intensive care and palliative care, then moved to study in Sweden, where she met her husband before they moved to the UK three years ago.
Leila, a lecturer at Edinburgh Napier University, said: “I became pregnant for the first time when I was in Sweden.
“I was completing a PhD in healthcare ethics, so I was already writing about issues like consent, shared decision-making and the importance of care that’s centred on a person’s individual needs.
“My pregnancy with my first child was very difficult, and I was depressed and in great pain throughout. I asked the Swedish hospital staff for a C-section but was denied that option, and was coerced into having a very traumatic induction.
“When that didn’t work, the clinicians relented, and I had a caesarean, but what happened before and after it was horrendous – there was no proper attempt to explain what they were doing to my body or to genuinely get my consent for anything, including intimate examinations and very painful procedures.”
Leila said she should have received person-centred care but instead suffered what is referred to as “obstetric violence”, a term that can include the disregard of a pregnant woman’s needs and pain, denial of care, invasive practices, forced medical intervention and dehumanising treatment.
Leila said she was diagnosed with post-traumatic stress disorder (PTSD) after her first daughter’s birth and waited over five years to have her son, by which time she’d moved to the UK.
She explained that the experience of giving birth for a second time only added to her trauma, as there was resistance to elements of a birth plan developed to take account of her PTSD, such as her need to avoid particular intimate procedures and obtaining consent for interventions and care.
She says that, when she went to the hospital for her c-section, there was a lack of awareness of the plan’s contents, and the most crucial aspects of the birth plan were breached or not implemented.
“I was so traumatised that I couldn’t bond with my son for a year, and I was in that state when I unexpectedly became pregnant with Aurora,” she recalled.
“I knew I had to have a maternal-assisted c-section this time, along with safeguards and guarantees on my needs for respectful care – appropriate informed consent, shared decision making and protecting my dignity during birth.
“I was delighted when the NHS Lanarkshire team agreed to the maternal-assisted option and my other needs and wishes, and we had multiple discussions and a full simulation session using a doll – a first for the clinicians.
“When she was being born, the lead obstetrician brought Aurora’s head and shoulders out, and I then completed the birth by grasping her under her arms and lifting her onto me.
“The team was also marvellous in accommodating a list of my requests, which included no announcement of the baby’s gender, lights dimmed after I lifted her, and a quiet moment to speak to Aurora so that my voice was the first one she heard. But I ended up uncontrollably sobbing with joy.
“I was also able to keep her on my chest to continue skin-to-skin as I was transferred from the operating theatre to the ward.
“My recovery was very easy compared to the previous C-sections. Aurora and I had no complications, and we were able to go home the very next day.
“Aurora is a healthy and happy ten-month-old who is the light of our world.”
Trudi Marshall, NHS Lanarkshire executive nurse director, said: “We’re immensely proud of our maternity and obstetrics colleagues for the way they stepped out of their comfort zone to offer Leila the opportunity to give birth in the way she wanted and needed.
“It’s a fantastic example of what we strive to provide – care that’s person-centred and trauma-informed and reflects Scotland’s health and social care policy of Getting It Right For Everyone.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country