A midwife insisted there were “no red flags” when a pregnant woman was examined the day before going into labour with an undiagnosed breech baby who later died, an inquiry heard.
Mirabelle Bosch died aged just 12 hours on July 2 2021 at Wishaw General Hospital when life support was withdrawn, after she suffered a hypoxic brain injury during a home birth and there was a delay taking her mother, Rozelle Bosch, 31, to hospital.
A fatal accident inquiry into her death will also examine the deaths of two other newborns in NHS Lanarkshire hospitals: Ellie McCormick, who died at the same hospital aged just five hours on March, 5 in 2019; and Leo Lamont, who died at two hours old in University Hospital, Monklands, on February, 15 in 2019.
Medics believed Mirabelle was head-down in a “low risk” pregnancy. However, she was actually in breech, which would require a management plan for a a hospital birth due to head injury risks for the baby.
A 31-week scan identified Mirabelle was in breech but a midwife gave evidence and said this was not a cause of concern at that time.
First-time mother Mrs Bosch had no concerns throughout her pregnancy and Mirabelle appeared healthy, but when labour began, her feet emerged rather than her head, which became “entrapped”, causing her death, the inquiry heard.
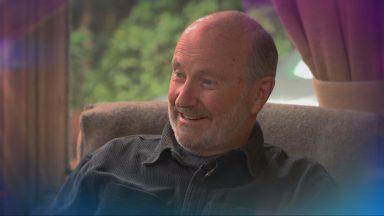
On June 30, midwife Michelle Tannahill examined Mrs Bosch, who had attended Wishaw General after her waters broke, and was then sent home with no formal written guidance from the NHS about active labour.
Ms Tannahill told the inquiry at Glasgow Sheriff Court a vaginal examination could “possibly” have found the baby was in breech but would have been avoided due to the risk of infection, and she said there was no reason for her to seek a second opinion as she believed she could feel the baby’s skull.
“From my assessment of it, I determined it was a head that I was feeling at the brim and the buttocks at the top. I had no difficulty when I was listening into the heartbeat at all, there was no difficulty picking up the heart,” she said.
“From what I was feeling above the brim of the pelvis, I felt that was the head, normally a bony prominent part rather than soft buttocks.
“The head was not mobile, that’s how I came to the conclusion it was fixed in the pelvis. Above the brim of the pelvis I could feel four-fifths of the head. The colour of liquid was clear, there was no concerns over the baby’s movements.”
She added: “The midwives who work with risk management who carried out an extensive investigation into what happened and they did not see anything wrong with my practice.”
Ms Tannahill said she did not seek a second opinion from someone more senior or a referral for a scan because the situation was within her clinical area of expertise and there was no reason to be concerned.
She said: “No, there wasn’t any red flags, everything that I had found that night was within my scope of practice within midwifery. There wasn’t anything that was alarming.”
When asked if there was a leaflet which Mrs Bosch could have been given, Ms Tannahill said: “I am aware there’s an induction of labour pamphlet but, in terms of rupture of membranes, I’m not sure there’s a specific leaflet relating to that.”
Sheriff Principal Aisha Anwar asked if there was a “specific leaflet” which could have been given.
Ms Tannahill replied: “There possibly could have been, yes, but I’m not 100% sure if there was.”
An induction was booked for 9am on July 2 according to NHS Lanarkshire guidelines, but this guidance has now changed, the inquiry heard.
Mirabelle died three hours after this was due to take place at 12.15pm, when life support was withdrawn.
A statement from the baby’s father, Eckhardt Bosch, had questioned why no vaginal examination was carried out.
Ms Tannahill said: “You want to minimise any intervention which is unnecessary due to the risk of infection. There was no reason for me to examine – there was good reason to avoid doing one.”
She said a vaginal examination could “possibly” have determined the baby was in breech, but added: “I had no doubt about what I was feeling.”
Cross-examined by a lawyer from NHS Lanarkshire, Ms Tannahill said she had discharged Mrs Bosch with advice to contact the maternity triage if something changed.
She said: “Mrs Bosch knew when to phone initially, she knew the triage was there and why we were there. She was given the advice to call when she was discharged. Whenever you discharge someone home we say, if you have any concerns pick up the phone.’”
Retired midwife Alison Stark spoke to Mrs Bosch on July 1 at 2.29pm, the inquiry heard.
She said: “If a woman during the conversation seemed to be in pain or distressed, we would obviously suggest they would come to the unit.
“You couldn’t really determine if they were in active labour until they were seen, you could only go with what they were telling you on the telephone.
“There are many leaflets that are given, we also have an app which many people use on their phone which gives them a lot of information. I would say most women use the app on their phone.”
The inquiry was told that Mrs Bosch had declared she did not want oral pain relief during birth.
The retired midwife gave evidence and said “the option would have been given” to come into hospital when they spoke on July 1, hours before labour began.
Ms Stark said: “I think most people know whether they are managing pain relief on their own or not. It’s already been established Mrs Bosch declined oral medications. You do find women will be able to tell you if they wish to come for further assessment.
“The option would have been given to her to come to hospital at that point.”
A text message sent by Mrs Bosch to another midwife read: “Hello Lesley thanks so much for the well wishes, I phoned Wishaw Hospital five minutes ago as I have had contractions for past five hours. The individual who helped me said I should only come in when I couldn’t bear the process anymore.”
However, Ms Stark said this was a phrase she “would never use”.
She said: “I would never tell any woman not to come in. I would have told her even if she came into triage we could send her home afterwards and continue with the plan which was already in place.”
The FAI heard that three midwives are now on duty in the maternity unit.
The inquiry continues.
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country


 SNS Group
SNS Group