Each year, more than 8,000 new patients pass through the doors of the Beatson West of Scotland Cancer Centre to begin treatment for the disease.
On Tuesday morning, Michael Gault was about to have surgery to treat his prostate cancer performed by an expert team led by clinical director Dr David Dodds.
Michael, 57, was diagnosed in August 2024.
“You come in, and you just feel as if they’re friends,” Michael explained. “There isn’t that ‘doctors, patient, nurse’ thing. You just feel as though you are all part of one unit.
“I’ve been really fortunate – I’ve come through the system at pace. I’ve been well looked after and supported by everyone.”
As Michael’s final pre-op checks took place, a young nurse buzzed around him, taking notes.
They joked about the weather, the early mornings – and the fact he agreed to a camera crew filming and broadcasting his prostate surgery, all while having a front-row seat.
 STV News
STV News“If I can help – I will,” he said as he signed the consent forms.
Afterwards, in theatre, Dr David Dodds and his team carried out brachytherapy or prostate seed implantation.
The surgery involves placing irradiated metal implants smaller than a grain of rice into the prostate gland to deliver a precise, high dose of radiation. It’s meticulously planned, with the team checking and then cross-checking each move.
It’s one of an increasing number of ways the disease can be treated, but there are concerns about the demand for services.
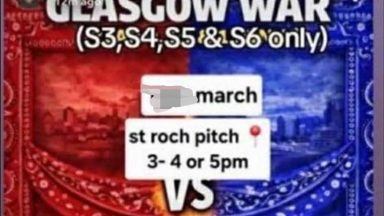
Dr Dodds explained: “Whilst there has only been a small increase in the total number of patients being referred, the number of treatments those patients are receiving has gone up, sometimes up by 70%.
“The problem is that the increase in demand has not necessarily been matched by an increase in the resource to furnish the demand, and that has created difficulties issues in the department as a whole.”
 STV News
STV NewsA total of 36,036 people in Scotland have been diagnosed with cancer in one year, according to the latest figures from Public Health Scotland.
While it’s only a small increase on the year before, it’s part of an upward trend that is placing increasing pressure on the NHS.
The data also shows a 30% increase in the number of men and women being diagnosed with colon, rectal and bowel cancers over a ten-year period.
The Beatson is at the forefront of research and treatment of the disease.
While the rise in new treatments is welcomed, they come at a cost. Chiefs say that beyond the pounds and pence is a demand for staffing, overtime and specialist training.
“A lot of drugs, when they are approved, they’re approved in isolation; there is a drugs cost, and that is what is expected to be met”, Dr Dodds added.
“But what is not met is the cost of the pharmacists, the nurses, the doctors the technicians, the admin staff and everything that goes along with running a service.
“So it would be a real improvement if we are able to incorporate a more holistic approach.
“I think we’ve been very successful in the past few years changing the way we work to mitigate against capacity problems we have.”
 STV News
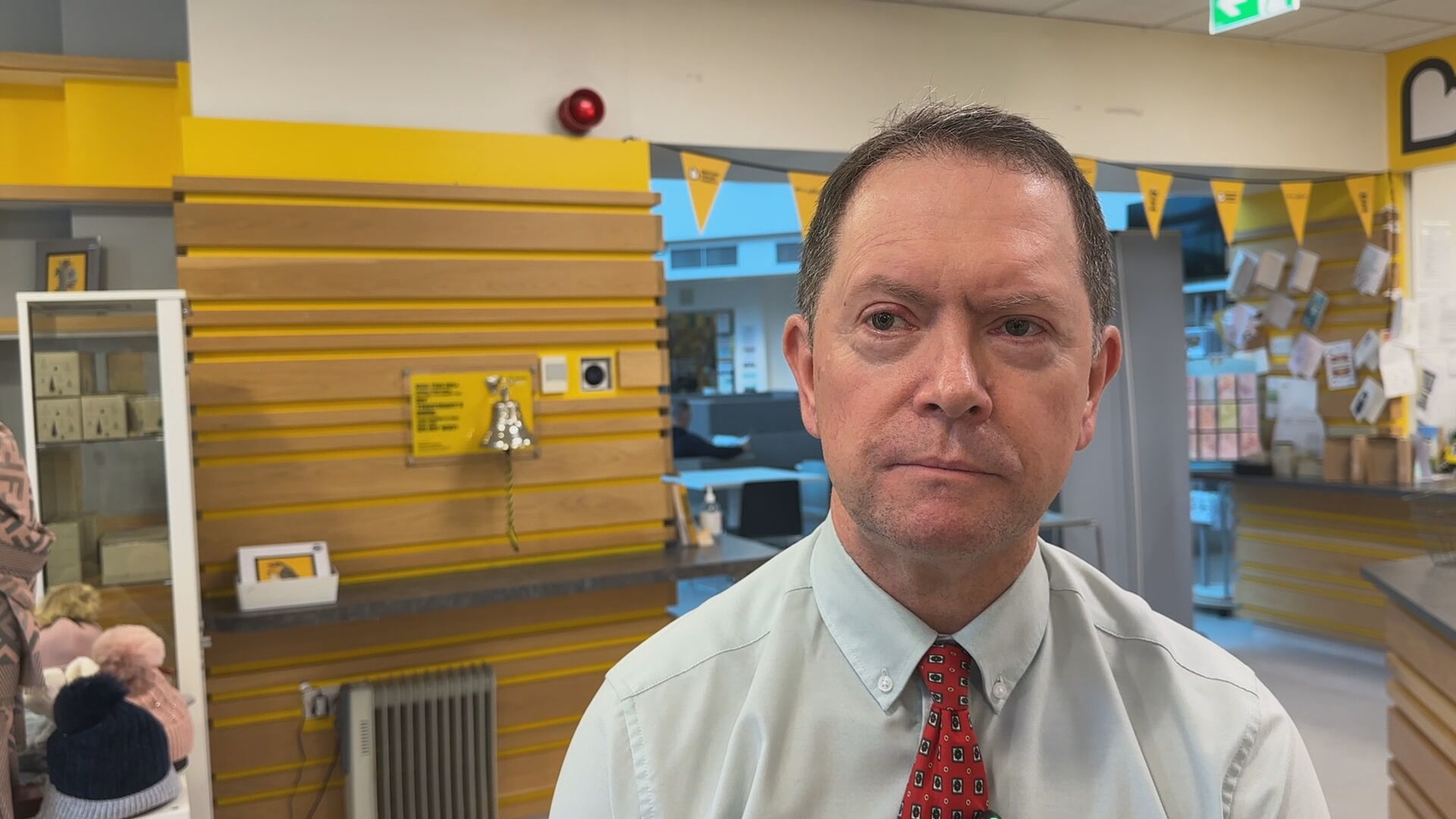
STV NewsAlongside the surgical, the Beatson also provides services to help patients cope as they go through treatment.
Upstairs at the Wellbeing Centre, patients can step away from the wards for a massage, haircut, wig fitting, or a catch-up with friends and family.
The centre manager, Claire, explained how they work closely with their colleagues throughout the hospital to provide appropriate support and care.
“The areas that we are focussing on are the additional things, like supporting people emotionally, providing light relief”, she said.
“So, if someone wants a chat or to get away from that ward environment, we’ve got activities, and we provide that place to get away from the ward which is really really important.”
Jane Tait is receiving treatment for cancer in her eye. On Tuesday, she sat chatting with a friend in a high-backed, comfy chair that wouldn’t look out of place in a high-street coffee shop.
The radio played, and the sun was coming through the high-glass windows, which looked out to Glasgow.
 STV News
STV News“It’s just wonderful. You walk in, and they ask if you want a cuppa. You get lots of them and biscuits, and your friends can visit you and sit here”, she said.
“You feel like you’re in a café with lots of sky and roofs and views – it’s deliberately non-medicalised in here.”
The Beatson also offers a befriending service, providing one-to-one telephone companionship and regular contact.
Run by volunteer befrienders, they offer emotional support and highlight more practical resources available. It means patients and their families can get advice whenever they need it.
Marlyn Hosie, volunteer manager at The Beatson, explained: “Some of our clients that use the scheme might be surrounded by family, but they maybe don’t want to share too much for fear of upsetting them.
“On the other end of the spectrum we have clients that we have been phoning for a wee while who have nobody else to speak to. They’d go through all of that on their own if they hadn’t access our telephone befrienders.”
“Everything the volunteers do here is designed specifically to make patients and their loved ones feel cared for and cared about.
“It’s about working in tandem with NHS colleagues in a space between family and medical teams to bring comfort, kindness, hope and someone to talk to.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country