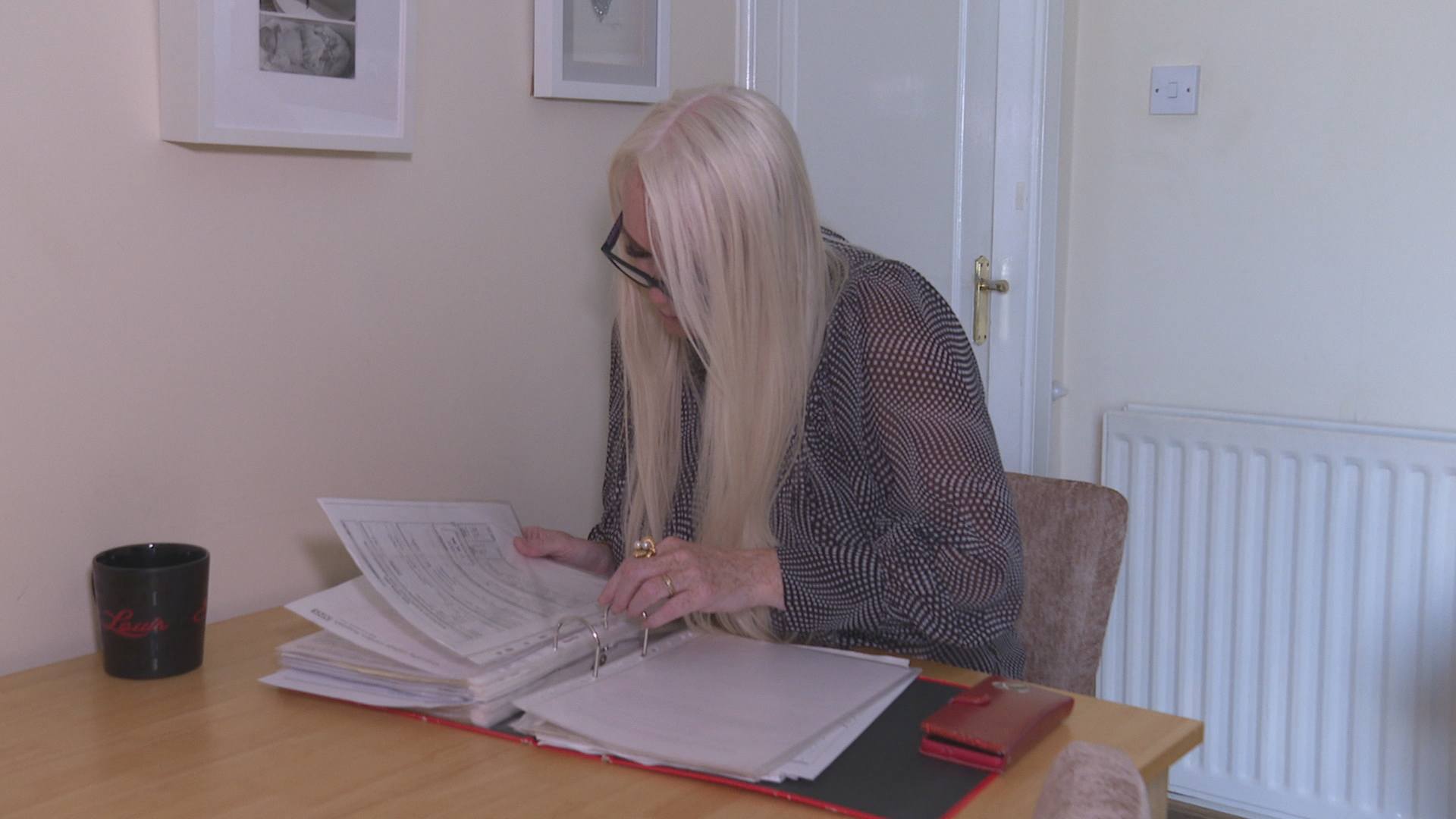
A woman harmed by a vaginal mesh implant has described her wait for follow-up surgery as “disgusting” – claiming she has been “maimed” by the NHS.
Nancy Honeyball, from Dunoon, had the implant fitted in 2010 due to bladder problems and says she has been “plagued” with complications ever since.
She is among many mesh-injured women who say they are still being failed by the Scottish Government.
Nancy travelled to Missouri in the US for removal surgery with renowned mesh specialist Dr Dionysios Veronikis in March 2024 under a scheme funded by the Scottish Government. She had hoped the operation would finally be the end of her ordeal.
She said Dr Veronikis was “shocked” to learn of her experiences.
“His words were ‘if that had happened in America, there would be a lawsuit,'” Nancy told STV News.
“He’s had a look as a professional and been quite upset at how they’ve been left. He looked at me and he said an animal would be treated better,” she said.
“I’m grateful I managed to get on the list to go to America, but I wouldn’t go as far as to say ‘thank you very much.’ The NHS maimed me – and thousands of others – all to save money. It’s always been profit over health, and it’s wrong.
“I don’t trust the surgeons in Scotland – that’s why I fought to go to the USA.”
 STV News
STV NewsIn the year since her operation, Nancy said she had no check-ups or calls from the NHS.
She added: “Even Dr Veronikis has been in touch numerous times to check how I am, but nobody from the NHS in Scotland has. I feel, after the way I was treated in Glasgow, that I’m blacklisted, and that’s why I’m having to fight so hard to get things done. It’s wrong.”
Nancy underwent her first surgery to remove a transvaginal mesh implant in London in 2017, but it was unsuccessful and failed to resolve her chronic pain.
In 2019, she had a second surgery in England to remove the mesh arms. Despite making it clear that she did not want any more plastic implanted, Nancy was horrified to discover that plastic sutures had been used.
Her complaint to the the General Medical Council resulted in a Medical Practitioners Tribunal in October 2024. The surgeon involved was suspended for nine months.
‘I’ve been plagued by this for 15 years’
Dr Veronikis successfully removed Nancy’s remaining mesh in March 2024, but was unable to take out the sutures due to limits in the Scottish Government’s contract, which covered only mesh removal, not full pelvic repair.
Back in Scotland, Nancy was referred to Crosshouse Hospital in Kilmarnock. However, she received a letter from NHS Ayrshire & Arran informing her she would face a 92-week wait for further treatment.
“I had a total meltdown. I had a panic attack.. Because it’s just too much. Why should a patient have to chase and chase follow‑ups? It’s ridiculous.
“People might think, ‘who do you think you are? Everyone else has to wait.’ When you’ve waited and fought for nearly 15 years – that’s how long I’ve been plagued by this – I wish I could turn the clock back.
“If I’d seen the device they use, I’d never have gone with anything. I’d say ‘no thank you – I’ll stay how I am.’
“But you trust the doctors. We were told it’s a gold standard operation, and you’d be in and out the same day. It would change your life forever. It certainly did; it changed my life for the worse, not the better.”
Over two decades, more than 20,000 women in Scotland had transvaginal mesh implants to treat post-childbirth conditions, like incontinence and prolapse.
Its use was stopped in 2014 after hundreds of women were left with painful, life-altering complications.
In 2021, then health secretary Humza Yousaf, announced contracts for mesh patients to undergo removal surgery from Dr Veronikis in Missouri or Spire Health Care in Bristol through the National Mesh Removal Referral Pathway.
Figures show that 64 patients have now travelled to independent providers in England or the United States for mesh removal surgery, at a cost of around £2m to the Scottish Government.
Since April 2020, 339 patients have been referred to the Complex Mesh Surgical Service in Glasgow and 161 have undergone surgery.
A spokesperson for NHS Greater Glasgow and Clyde said that while some of the remaining patients may still be undergoing assessment, the majority are either receiving conservative (non-surgical) treatment, have opted not to proceed with surgery, or were found not to require it.
A separate £1m fund was set up to offer women a one-off payment of £1,000 to help towards the costs associated with emotional or practical support.
Nancy branded the fund “a slap in the face” and said a full redress scheme is needed.
“There are so many things mesh has affected – loss of jobs, houses, marriages, relationships. People are left to fend for themselves,” she said.
“To me, everything should be covered. The NHS maimed us – it’s the biggest scandal since Thalidomide and the blood scandal. Nobody has been brought to justice. I don’t understand.”
Nancy now has an appointment scheduled for next month, but she remains in pain and emotionally exhausted.
“It’s been a constant rollercoaster, emotions up and down. Some days I totally break down. I’m a strong, independent person – I’ll be laughing and joking, but it’s just a mask.
“People will say, ‘I don’t know how you’re still standing’ – but I’ve got to keep fighting. Even though I just want to give up. I keep going.”
 STV News
STV NewsWomen’s health minister Jenni Minto said she has been working closely with Scottish Government teams to improve support and aftercare for those affected.
She said: “It’s important to recognise the Scottish Government has supported women to allow them to get their mesh removed. I do appreciate that some women have not had the right support once that has happened.
“We expect the local health boards to take that responsibility and look after women. Because after having had that treatment, the best place to continue the support and the ways that they can improve the way they’re living their lives is as locally as possible. I expect local health boards will be doing that.
“I’m working very closely with NHS Education for Scotland (NES) to ensure that is spread out across health boards so they do recognise the importance of that.
“But I also think we have to recognise this is quite a complicated situation and, therefore, we need multi-disciplinary teams and the right ones in the right place to be able to support women to heal – and hopefully return to a better life.”
A spokesperson for NHS Ayrshire and Arran said: “We cannot comment on individual clinical cases due to patient confidentiality.
“The COVID-19 pandemic created significant challenges and backlog of women requiring both urgent and routine treatment. Our waiting times for the gynaecology specialities increased significantly as women had not had the routine screening or treatments in primary care as per usual patient pathways during the pandemic.
“As a result the health board have focussed on the key areas of high demand with planned reduction in waiting times. Urgent and cancer diagnostic pathways are prioritised and we have increased available capacity by developing nurse-led services to address service demands and improve timeous access for our patients.
“We don’t underestimate the effect these conditions have on women’s quality of life, in particular ones affected by mesh complications. There are improvement plans in place within Uro-gynaecology and we are working towards reducing our waiting times to no more than 52 weeks by the end of March 2026.
“NHS Ayrshire & Arran acknowledge the impact of the extended waiting times on our patients and their health.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country