Nurses feel overwhelmed by the workload, trying to prevent infection and battling coronavirus itself, frontline workers have warned.
Claire McPake, the senior charge nurse for the Acute Medical Unit at the Royal Alexandra Hospital in Paisley, said that although staff have been given support, they are tired.
STV News was given special access to the hospital as health chiefs try to stress the importance of following lockdown rules.
Earlier this month, senior medics at Monklands Hospital and nurses from across Scotland said the health service was “on the edge” as it tried to cope with the crisis.
Ms McPake said: “We are always busy at this time of year, and after Christmas or New Year. It has been particularly worse this year.
“People are not being discharged as early as they would normally be.
“They are all being seen, but there is bit of a delay getting patients home so there is a delay getting patients in.”
The Acute Medical Unite receives patients from A&E and from the newly established SATA (Specialist Assessment Treatment Unit).
Ms McPake said that only patients with a negative test are supposed to come from SATA, and they are then placed into big rooms.
But if a person is then discovered to have Covid, the room has to be carefully cleaned before it can be used again.
She said: “Yesterday we had a patient in [a] big six-bedded area, who came in and had symptoms on an X-ray.
“This is a coincidental finding, and we decided this patient probably had Covid.
“So this becomes what is known as a contact bay, because there are already other patients there, so if anyone gets moved out or goes home, we have to keep those beds closed.”
The nurse said the contact patient gets moved to a single room and the room gets cleaned, meaning there are others on trolleys in A&E that cannot come in because there is no space.
In order to make the room safe again, staff must strip the beds, wash them down and then remake them.
Ms McPake said it can be a “vicious circle… if you’ve not got enough bodies on the floor”.
The nurse had Covid herself back in April. She lost her sense of taste and smell, and the latter has still to return.
Claire Harrow, clinical director for medicine, said: “Staff are exhausted. They’re unwell. A lot of them have either had Covid or have had relatives who have had Covid. They’ve got their own personal pressures.
“We’ve got parents, children, loved ones, all those stresses and strains that other people have. In addition to that uncertainty, and also the anxiety about what we’re doing… but also what we’re not doing.”

Ms Harrow, who has been in her post for two years, said her duty to look after patients and staff has never been been more important, but that the relentless pressure was taking its toll.
She said: “It’s not a simple illness, it’s not flu, everyone gets it slightly differently, so there are people who will bounce back quickly but there are other people who are really quite severely affected in many different and unpredictable ways.
“We can’t just expect that once someone’s Covid leave is up they’re going to be able to bounce back and step back in.”
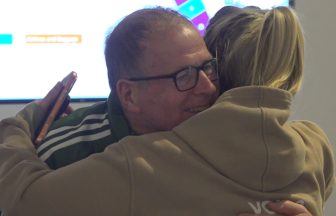
On the ward, Ms McPake described how a lack of face-to-face interaction with relatives of patients has made the job emotionally draining.
She said: “We have end-of-life patients. That’s been very, very difficult on the nursing staff. That’s what I find most challenging.
“The end-of-life relatives and trying to let relatives in, and trying to limit the number of relatives coming in through the door.
“If it was my mum, I’m one of four, we would all want to go in and visit my mum.
“It’s very difficult if you’ve got a big family and you’re trying to say to people you can only have one relative to come and visit.”
Additional reporting by Gianni Marini
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country