Self-managing pessaries cause fewer issues in women with pelvic organ prolapse, a new study has shown.
The six-year £1.1m study, Treatment of Prolapse with Self-Care Pessary (TOPSY), involved 340 women of all ages from 21 NHS centres across the UK and the results could change the lives of thousands of women with pelvic organ prolapse.
Research has shown that self-management of a pessary used to treat pelvic organ prolapse in women leads to fewer complications and could save the NHS money while maintaining quality of life.
In the UK, most women who use a pessary attend clinics for their care and have to return every six months for check-ups.
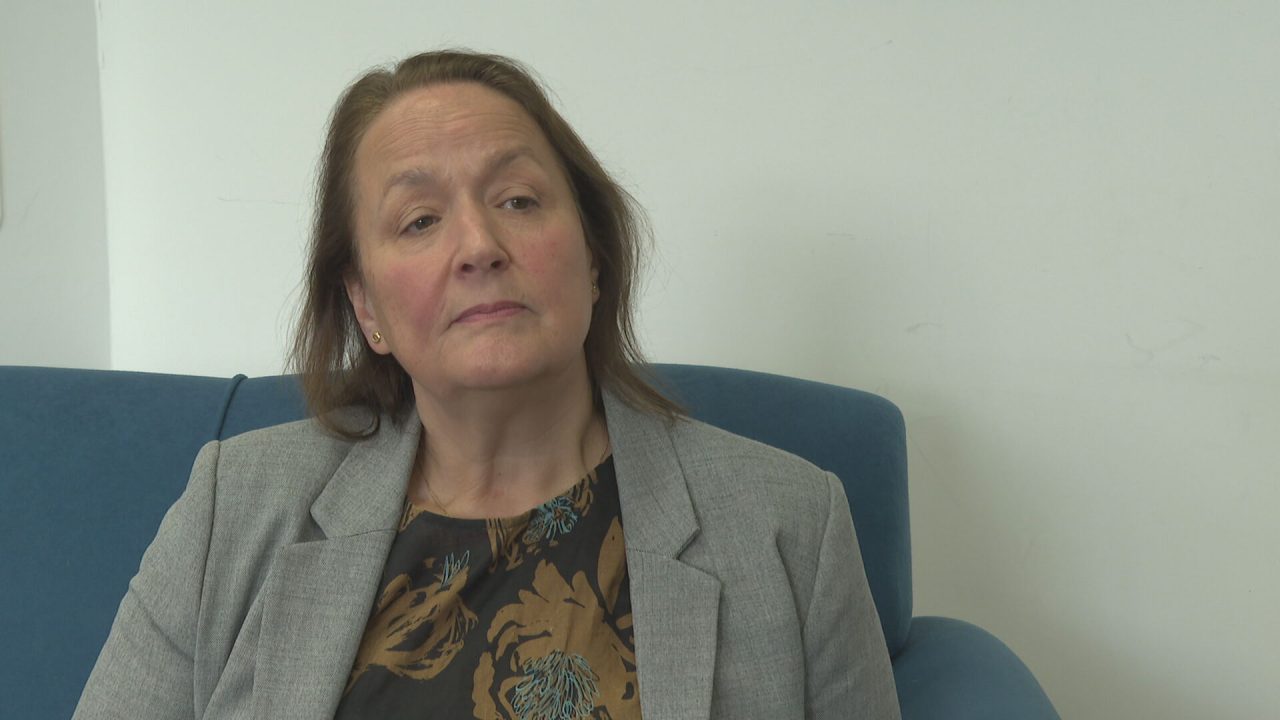
However, lead researchers Professors Carol Bugge and Suzanne Hagen at Glasgow Caledonian University have identified big benefits from pessary self-management.
Professor Hagen said: “This was a very large unique trial and the first in its field.
“We were looking for effective treatments for women which did not involve surgery. Not every woman is suitable for surgery. Alternatives are needed. What else is available, what can nurses and physiotherapists provide for women.

“Around 30% upon examination will have it and around 10% will have significant symptoms.
“We’re trying to see women treated in hospital as an outpatient versus managing it alone and what the differences are.
“The study explores whether they need to go back and forward to hospital and can they self manage the pessary to fit in with their way of life.
“It was a fully-powered trial with enough participants involved to give us robust answers. It was also diverse in terms of the age ranges of the women involved and their geographical location within the UK.”
Pelvic organ prolapse is a common condition in women.
It sees one or more of the organs in the pelvis slip down from their normal position and bulge into the vagina.
One treatment option for prolapse is a vaginal pessary, which is inserted into the vagina and holds the prolapsed organs back in place.
It is hoped women will eventually be able to self-manage their pessary as routine practice across the UK but more research is needed into how it can be made routine practice.
Professor Bugge said: “This research is great news for women in the UK who suffer from prolapse because it shows that women can safely self-manage their pessary from home.

“No matter their age, they may experience fewer complications and there will be less cost to the NHS in the long-run by freeing up appointments.
“Pessaries are a very commonly-used treatment in the NHS and the mainstay of treatment is that women have to return to clinics roughly every six months, which can be inconvenient and costly.
“This is why we have been looking into self-management for women. Our belief is that by giving the control of their health back to the women it would make their quality of life better.
“We are reaching out to women and healthcare professionals who provide pessary care with these results, so they can see that self-management is a valid option for them. It offers safety, it doesn’t worsen their quality of life, there are fewer complications and for services, it costs less and it frees appointments.”
Margaret Graham, 63, from Ayrshire, who has been using a pessary for the past ten years for prolapse and was a patient representative in the study.
Margaret said: “I was really delighted when I was presented with the option of a pessary for this condition.
“I was gobsmacked that this simple silicone donut-shaped thing worked. I thought the only option was surgery and it was terrifying.
It’s so easy to use. I can put it in and take it out when I need it. It makes me feel comfortable.
“I can go to an exercise class and not feel too worried.
“Vaginal prolapse is a very unpleasant sensation. it’s a feeling of something coming down.
“It’s so important that women are presented and supported with as many options as possible for what can be nearly another half of their lives.
“The results of this study could really change thousands of women’s lives if a self-management programme was rolled out because it’s safer, has less complications and stops the need to attend clinics as often.”

Professor Andrew Farmer, Director of NIHR’s Health Technology Assessment (HTA) Programme which funded the research, said: “These findings will undoubtedly be hugely encouraging for the many women affected by pelvic organ prolapse.
“The results once again highlight the continued contribution of evidence from high-quality independent research in transforming health and social care treatments and practice.”
The trial involved a large collaborative team including Chief Investigator Professor Bugge and co-Chief Investigators Professor Hagen, from the University’s School of Health and Life Sciences’ Nursing, Midwifery and Allied Health Professions Research Unit, and Dr Rohna Kearney, of Saint Mary’s Hospital at Manchester University NHS Foundation Trust.
Minister for the Women’s Health Strategy, Maria Caulfield, described the research findings as “an important step for women to manage their ongoing care for pelvic organ prolapse in the comfort of their own homes. It means women can continue to live their lives as usual and reduces the need for frequent visits to see clinicians.”
She added: “We recently announced a nationwide pelvic health service, backed by £11m, to come into effect in 2024, while a £25m investment into women’s health hubs is already improving access to diagnosis and treatment for conditions including pelvic organ prolapse.
“Research is a core part of our first-ever Women’s Health Strategy for England and is why between April 2022 and July 2023 we invested £53m into the NIHR to focus specifically on research into women’s health issues.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country