Scotland is facing a “bleak situation” in terms of GP care, ministers have been warned, as a survey found a quarter of family doctors are considering quitting in the next two years while more than two-fifths of practices cannot meet demand from patients.
A survey by the British Medical Association (BMA) of GPs in Scotland found just one in 20 (5%) of those who responded believe their practice is in a long-term sustainable position.
Meanwhile, three out of five (60%) said they feared for the future of their practice if it was to lose a GP.
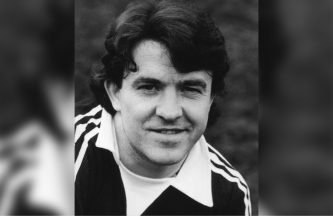
BMA Scotland GP chair Dr Andrew Buist warned without “urgent action” from the Scottish Government parts of the country could “become seriously under-doctored”, resulting in patients struggling “even more than they are right now to get appointments”.
The medic insisted: “The Scottish Government must take this situation seriously and show greater willingness for increased investment in core general practice services to maintain stability.”
As well as “concerted action” to recruit more GPs, he said there must also be action to retain existing doctors, with Dr Buist stating: “It is no good recruiting 20 if you lose 25 in the process.”
His comments came as the survey showed 43% of GPs in Scotland believe there is no realistic chance in the near future of their practice being able to meet patient demand for access, according to the survey.
More than a quarter (28%) of GPs said their workload was unmanageable, with 85% of family doctors saying they sometimes or regularly struggle to cope, and that their work is having a negative impact on their physical and mental wellbeing.
More than 850 doctors in Scotland took part in the survey, with Dr Buist saying the results “show once again just how precarious the position is for practices and GPs themselves across Scotland”.
He stated: “It is a very bleak situation and already many GPs fear the practices they work in are simply not sustainable in the long-term – leading, of course, to further worry for patients about accessing care, and continuity of care.
“Significantly, our survey suggests this is only going to get worse given the current direction of travel, with a quarter of GPs saying they will leave their current practice in the next two years, and three-quarters saying the last year has made them more likely to leave the profession altogether.
“That paints a very worrying picture for the future of GP services.”
He told how the “current demanding situation” was “taking its toll” on GPs across Scotland.
Dr Buist said: “Concerningly, 85% of those who responded to this survey said they sometimes or regularly struggle to cope, and that work is having a negative impact on their physical or mental wellbeing.
“That is a dreadful statistic and I want every doctor out there who is feeling this way to know they are not alone and there are support services available through the BMA, regardless of membership.”
With more than two-fifths of GPs saying their practice cannot meet current levels of demand, he warned the “unmanageable workloads and deteriorating work-life balance” could see more doctors leave.
Dr Buist said: “All of this suggests a position that is likely to get much worse, with practices collapsing, handing back contracts and patient care suffering as a result.
“Without urgent action, we will see parts of Scotland become seriously under-doctored as many patients will struggle even more than they are right now to get appointments.
“This will lead to deteriorating continuity of care, something patients greatly value, and the potential for the breakdown of primary care in those areas.”
Calling for action from the Scottish Government, he said there needed to be a “proper funding uplift”, alongside an “urgent review” of the target set by ministers to recruit an additional 800 GPs by 2027.
This work is needed to see the “progress or lack of” towards the target and “what must be done to get us back on track”, Dr Buist said.
A Scottish Government spokesperson said: “We are grateful to GPs for the vital service they provide and thank them for their efforts in the face of sustained pressure.
“GPs can access a range of resources, including the national wellbeing hub, a 24/7 compassionate listening service, confidential mental health treatment, coaching for wellbeing and psychological therapies.
“We have delivered a record number of GPs working in Scotland, with more per head than any other country in the UK, and we are making good progress on our commitment to recruit at least 800 new GPs by 2027. Since 2017, Scotland’s GP headcount has increased by 291 to a record high of 5,209 in 2022.
“To support general practice we currently have 4,731 staff working in multi-disciplinary teams providing services including physiotherapy, pharmacy and phlebotomy, giving an average practice access to more than five additional multi-disciplinary team members.
“We continue to support development of these teams through our investment of £170m per year in the Primary Care Improvement Fund.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country


 PA Media
PA Media