An Edinburgh woman is celebrating being free from bowel cancer and said she “wouldn’t be here” without her life-saving stoma.
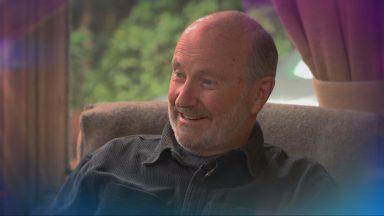
Jillian Matthew, 50, is fighting fit and has been travelling abroad with her husband three years on from her devastating diagnosis.
The public sector worker experienced a change in her bowel habits for a few months and, when she saw blood in her poo in February 2020, went to see her GP.
She said: “You panic a bit when you see blood – it’s not meant to be there.”
Jillian was given the news she had bowel cancer in March 2020 and was admitted to Spire Murrayfield Hospital for surgery to remove her rectum three weeks later during the height of Covid restrictions.
During the surgery she was given a stoma, which is an opening on the surface of the abdomen created to divert the flow of faeces or urine, to replace the function of her rectum.
Tests after the surgery showed that the cancer had spread into her lymph nodes, which had also been removed as standard practice with bowel cancer, indicating the surgeon had managed to remove all the malignant material.
Three years later, she is living cancer-free and has adapted to life with a stoma.
She said: “It’s not something I would have chosen to have but I wouldn’t be here without it.
“I have a science background so I had researched it and I was given support of a stoma nurse who talked me through what it would be like.
“But you don’t know what it’s like until you have it.”
Because the cancer had been found in her lymph nodes, Jillian also underwent chemotherapy to ensure the cancer wouldn’t spread.
She said: “Six weeks after the surgery I was feeling good, but with the chemotherapy it took a further three months for the bowel to settle down.
“There are a lot of myths about having a stoma – that you can’t eat certain things, but I eat most things although I avoid beans and certain veg.
“You do have to plan a little more, no small handbag for me as I need to take spare supplies with me and finding accessible toilets which have a shelf, hooks and a sink is really important.
“But I still live my life as before, I’ve travelled and been through airports – something I was worried about and it was absolutely fine.”
Jillian has resumed running, walking the dog and even regularly does Pilates which focuses on strengthening core abdominal muscles.
She added: “You just have to be careful and adapt the exercises but I’m doing pretty much everything I was doing before. I am just really grateful given Covid that I was able to get the treatment I needed.”
It comes as a groundbreaking new technology to better target bowel cancer has been discovered by Cancer Research scientists in Glasgow.
Microbubble technology would see bubbles of a safe gas injected into the bloodstream of patients to identify which areas the cancer has spread to before examination using ultrasound – reducing the need for bowel cancer patients to have life-changing operations.
Currently surgeons are required to remove a significant amount of tissue surrounding a bowel tumour to try to remove the cancer and prevent spread of the disease.
However, only after removal can the tissue be analysed and confirmed as cancerous and sometimes the extent of this surgery leads to patients requiring a stoma and colostomy bag.
Jillian welcomed the pioneering new technology and said it was a step forward for treating bowel cancer.
She added: “This new research wouldn’t have helped me avoid needing a stoma due to where my cancer was located, but any focus on bowel cancer that can help future patients is welcome.”
The new research, published in the journal, Cancers, found that injecting microscopic bubbles into mice carrying bowel cancer tumours made ultrasonic identification of cancer-carrying lymph nodes easier.
The research team includes colorectal cancer surgeon Professor Susan Moug of the Royal Alexandra Hospital, Paisley; colorectal cancer geneticist Professor Susan Farrington and medical physicist Professor Carmel Moran both of the University of Edinburgh.
Lead researcher Dr Helen Mulvana, of Strathclyde University in Glasgow, said: “Current practice is for a substantial amount of surrounding tissue to be removed alongside bowel cancer tumours.
“This can lead to patients requiring a stoma which is a lifechanging procedure requiring an extensive recovery and adaption period.
“Our hope is that using microbubbles could allow doctors to see which tissue is cancerous during surgery and allow them to remove only what is necessary.
“This could reduce the extent of surgery, reduce the need for a stoma in many patients, and speed up the post-operative recovery time.”
Follow STV News on WhatsApp
Scan the QR code on your mobile device for all the latest news from around the country